STEM activities for preschoolers are playful, hands-on experiences that introduce science, technology, engineering, and math. They spark curiosity, build problem-solving skills, and lay the foundation for lifelong learning, fostering a love for discovery and exploration from an early age.
What Are STEM Activities?
STEM activities are engaging, hands-on experiences that integrate science, technology, engineering, and mathematics. These activities are designed to foster curiosity, creativity, and critical thinking in young children. They often involve exploration, experimentation, and problem-solving, using everyday materials to make learning fun and accessible. STEM activities for preschoolers are play-based, allowing children to discover concepts naturally through interaction and inquiry. They introduce foundational skills in areas like observation, sorting, building, and prediction, while encouraging children to ask questions and seek answers. These activities are simple to set up and require minimal resources, making them ideal for both classrooms and home environments. By focusing on process over outcome, STEM activities help preschoolers develop a mindset of experimentation and innovation from an early age.

Why STEM for Preschoolers?
Introducing STEM to preschoolers is essential for building a strong foundation in critical thinking, problem-solving, and creativity. These skills are vital for future academic success and real-world applications. By starting early, children develop a natural curiosity and confidence in exploring the world around them. STEM activities also enhance spatial awareness, fine motor skills, and collaboration, preparing young minds for an increasingly technology-driven world. Research shows that early exposure to math and science concepts can lead to higher achievement in these subjects later in school. STEM fosters a growth mindset, encouraging children to view challenges as opportunities for learning and growth. This early exposure not only sparks an interest in these fields but also equips children with essential life skills, making it a valuable investment in their educational journey.
Benefits of Early STEM Education
Early STEM education offers numerous benefits, fostering curiosity, creativity, and critical thinking in young children. It enhances problem-solving skills, spatial awareness, and fine motor abilities, while introducing foundational concepts in science, technology, engineering, and math. STEM activities encourage children to explore, experiment, and learn through trial and error, promoting resilience and a growth mindset. These experiences also improve collaboration and communication skills, as children often work in groups to complete challenges. Research indicates that early exposure to STEM can lead to better academic performance in later years and a stronger interest in these fields. By engaging in hands-on, age-appropriate activities, preschoolers develop essential skills that prepare them for future success in both school and the modern, technology-driven world. Early STEM education lays a strong foundation for lifelong learning and exploration.

Science Activities for Preschoolers
Science activities for preschoolers include nature exploration, plant growth experiments, and water cycle observations. These hands-on experiences encourage curiosity, observation, and early scientific thinking, fostering a love for discovery and experimentation.
Nature Exploration and Sorting Activities
Nature exploration and sorting activities are excellent ways to engage preschoolers in STEM learning. These activities involve collecting items like leaves, rocks, and flowers, which children can sort by shape, color, or texture. This hands-on approach introduces basic scientific concepts, such as observation and classification. For instance, teachers can create a classroom chart where children categorize their finds, encouraging critical thinking and an appreciation for the natural world. Sorting games also enhance fine motor skills and spatial awareness. Additionally, these activities can be extended by discussing the habitats and purposes of the collected items, fostering a deeper understanding of biology and ecology. Such experiences are not only educational but also foster a sense of wonder and connection to the environment, making learning fun and interactive.
Plant Growth and Observation
Plant growth and observation activities are a wonderful way to introduce preschoolers to the wonders of science and biology. By planting seeds and monitoring their growth, children learn about the life cycle of plants and the factors that affect their development. Teachers can guide students in recording their observations through drawings or simple charts, encouraging critical thinking and curiosity. These activities often involve experimenting with different conditions, such as varying light exposure or water amounts, to see how they impact growth. This hands-on approach fosters an early understanding of scientific inquiry and responsibility. Additionally, it sparks an appreciation for nature and the importance of caring for living things. Such experiences are both educational and engaging, making STEM concepts accessible and fun for young learners.
Water Cycle Experiments
Water cycle experiments offer preschoolers a fascinating look into Earth’s natural processes. Activities like creating a mini-cloud in a jar or building a DIY rain gauge help children visualize how water moves through evaporation, condensation, and precipitation. These hands-on experiments introduce basic concepts of meteorology and the states of matter. By observing water droplets, predicting weather changes, and measuring rainfall, young learners develop scientific observation skills. Such experiments are simple, engaging, and perfect for sparking curiosity about the environment. They also align with early STEM education goals by promoting critical thinking and an understanding of the world’s water systems. These activities are both educational and enjoyable, making complex concepts accessible to young minds while fostering a love for scientific exploration.

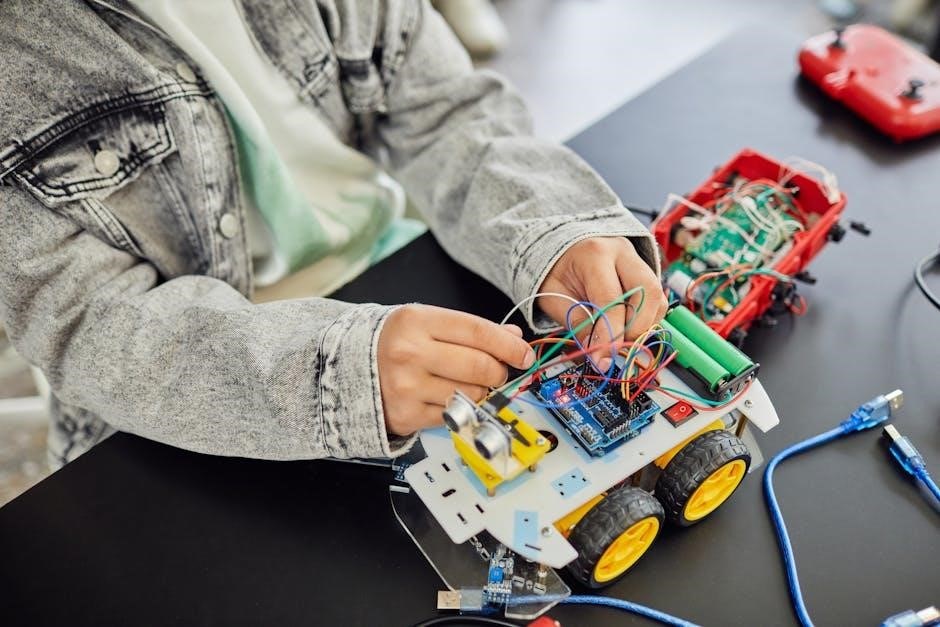
Technology Activities for Preschoolers
Technology activities engage preschoolers with simple tools, coding basics, and digital art, fostering creativity and problem-solving skills while introducing foundational tech concepts through playful, interactive experiences.
Introducing preschoolers to simple tools and gadgets fosters an understanding of technology’s role in everyday life. Using basic tools like magnifying glasses, flashlights, or scissors helps develop hand-eye coordination and fine motor skills. These gadgets encourage curiosity and exploration, teaching children how objects function and interact. For instance, using a magnifying glass to examine objects introduces the concept of magnification, while simple mechanics like gears or levers in toys demonstrate cause-and-effect relationships. This hands-on approach makes learning engaging and accessible, laying the groundwork for more complex technological concepts in the future. It also enhances problem-solving abilities and creativity, essential skills for STEM exploration.
Basic Coding Concepts Through Play
Introducing coding to preschoolers through play simplifies complex concepts into fun, engaging activities. Using blocks, puzzles, or sequencing games, children learn logic and problem-solving skills. Activities like arranging toys in a specific order or following directions to create patterns lay the groundwork for understanding algorithms. Digital tools, such as simple coding apps with visual blocks, further enhance these skills. These playful methods teach cause-and-effect relationships and critical thinking, preparing young minds for future STEM challenges. By making learning interactive and enjoyable, coding concepts become accessible and exciting for preschoolers, fostering creativity and curiosity from an early age. This approach ensures a strong foundation for more advanced coding skills as they grow.
Digital Art and Creativity
Digital art and creativity are vibrant components of STEM education for preschoolers, blending technology with self-expression. Using tablets, drawing apps, or interactive software, children explore colors, shapes, and patterns while developing fine motor skills. These tools allow young artists to experiment with digital brushes, animations, and layered designs, fostering imagination and innovation. Combining physical materials like stamps or stencils with digital platforms enhances tactile learning. Such activities introduce basic design principles and encourage children to view technology as a creative medium. By merging art with STEM, these experiences promote critical thinking, visual literacy, and confidence, preparing preschoolers for a world where creativity and technology are deeply intertwined. This playful approach to digital art makes learning fun and accessible, nurturing future innovators and artists alike.

Engineering Activities for Preschoolers
Engineering activities for preschoolers encourage creativity and problem-solving through hands-on building experiences. Using blocks, LEGO, or recycled materials, children design and construct simple structures, fostering critical thinking and innovation.

Building Challenges with Blocks
Building challenges with blocks are a fun and effective way to engage preschoolers in engineering concepts. These activities encourage children to think creatively and develop problem-solving skills. By using blocks, LEGO, or other building materials, kids can construct towers, bridges, or other structures, learning about balance, stability, and design. Such exercises not only enhance spatial awareness but also improve fine motor skills. Teachers can set specific goals, like building the tallest tower or the strongest bridge, to make the activity more engaging. This hands-on approach introduces basic engineering principles in a playful manner, making learning both enjoyable and impactful for young minds.
Bridge Building and Testing
Bridge building and testing is an engaging STEM activity that challenges preschoolers to design and construct sturdy bridges using materials like blocks, popsicle sticks, or cardboard. This activity introduces basic engineering concepts such as weight distribution, structural integrity, and stability. Children are encouraged to test their bridges with toy cars or small weights to see how much they can hold before collapsing. Through trial and error, they develop problem-solving skills and learn about cause-and-effect relationships. This hands-on experience fosters creativity and critical thinking while making learning fun and interactive. It also helps build confidence as children see their designs succeed or improve based on their adjustments.

Designing Parachutes for Toys
Designing parachutes for toys is an exciting STEM activity that encourages preschoolers to explore concepts of gravity, air resistance, and drag. Using simple materials like tissue paper, plastic bags, or napkins, children create parachutes for small toy figures. They test their designs by dropping them from heights, observing how well the parachutes slow the fall. This activity introduces basic engineering principles, teaching kids to think about how different materials and shapes affect performance. Through trial and error, they refine their designs to achieve the best results. This hands-on experiment sparks curiosity about the natural world and helps develop problem-solving skills in a fun, engaging way.

Math Activities for Preschoolers
Math activities for preschoolers include counting games, shape sorting, and measuring exercises. These hands-on experiences introduce basic numeracy, spatial awareness, and problem-solving skills, fostering curiosity and critical thinking from an early age.
Counting and Sorting Games
Counting and sorting games are essential STEM activities for preschoolers, enhancing numeracy and logical thinking. Using everyday objects, children practice counting, categorizing, and comparing quantities. These activities prepare them for basic arithmetic and problem-solving, fostering a strong math foundation while keeping learning fun and engaging.
Shapes and Geometry Basics
Introducing shapes and geometry basics to preschoolers through hands-on activities is a fun way to develop spatial awareness and problem-solving skills. Using blocks, shape sorters, and cutouts, children learn to identify and name basic shapes like circles, squares, and triangles. Sorting activities, such as categorizing objects by shape, enhance their understanding of geometry. These exercises also refine fine motor skills and encourage creativity. By exploring 2D and 3D shapes, preschoolers build a foundation for more complex geometric concepts later on. Simple, engaging activities like tracing shapes or creating collages make learning shapes an enjoyable experience, fostering curiosity and a strong math foundation from an early age. These activities are essential for developing critical thinking and visual-spatial skills in young learners.
Measurement and Comparison
Measurement and comparison activities are essential for developing early math skills in preschoolers. Simple tasks like comparing the lengths of objects or sorting items by size introduce basic measurement concepts. Using rulers or everyday materials, children can explore how to measure and quantify their surroundings. For example, comparing the height of plants or the weight of different toys fosters critical thinking and problem-solving abilities. Group activities, such as lining up objects from shortest to longest, encourage collaboration and a deeper understanding of relative sizes. These hands-on experiences help preschoolers grasp fundamental math concepts while making learning fun and engaging. By incorporating measurement into play, children build a strong foundation for more complex math skills in the future.
Combining STEM Disciplines
Combining STEM disciplines creates engaging, comprehensive learning experiences for preschoolers. Activities like building bridges or designing parachutes integrate science, technology, engineering, and math, fostering critical thinking and problem-solving skills.
Hands-On Experiments
Hands-on experiments are a cornerstone of STEM education for preschoolers, fostering curiosity and a deeper understanding of scientific concepts. Activities like planting seeds, creating rain gauges, or freezing dinosaur toys in ice encourage children to explore, predict, and observe outcomes. These experiments introduce foundational ideas such as plant growth, weather patterns, and basic physics. By using everyday materials, these activities make learning interactive and accessible. They also promote critical thinking and problem-solving skills, as children experiment with different strategies to achieve desired results. Hands-on experiments create a sense of wonder and excitement, making STEM concepts engaging and fun for young minds. They lay the groundwork for a lifelong love of learning and exploration.
Outdoor STEM Exploration
Outdoor STEM exploration offers preschoolers a unique opportunity to engage with nature and learn through discovery. Activities like nature walks, scavenger hunts, and collecting leaves or rocks encourage observation and curiosity. Children can explore the outdoors to identify different types of plants, observe insects, or track changes in weather. Simple tools like magnifying glasses or binoculars can enhance their experience. Outdoor STEM also introduces basic concepts like ecosystems, seasons, and the water cycle. By connecting learning to the natural world, these activities foster an early appreciation for science and the environment. They also promote physical activity, teamwork, and creative thinking, making STEM accessible and enjoyable in a real-world context for young learners.

Additional Resources
Explore downloadable STEM activity guides and recommended STEM toys to enhance learning. These resources provide practical tools and materials for engaging preschoolers in fun, educational experiences at home or in the classroom.
Downloadable STEM Activity Guides
Downloadable STEM activity guides offer a wealth of creative and engaging ideas for preschoolers. These guides provide step-by-step instructions for hands-on experiments, games, and projects that foster curiosity and learning. Many include printable materials, such as worksheets, charts, and activity cards, to support STEM exploration. For example, guides like the Playful Inquiry Lesson Pack offer activities like “How Do Plants Drink?” or “Flowery Business,” which introduce basic scientific concepts through play; Additionally, resources like “Kide Science” lessons provide fun experiments, such as creating rainbows in jars or exploring shadow shapes. These guides are perfect for parents and educators seeking structured yet flexible STEM experiences for young children, making learning accessible and enjoyable at home or in the classroom.
Recommended STEM Toys and Materials
Engaging STEM toys and materials are essential for fostering creativity and learning in preschoolers. Building blocks, magnetic tiles, and LEGO sets are excellent for developing engineering and spatial awareness skills; Science kits designed for young children, such as those for growing plants or creating slime, introduce basic chemistry and biology concepts. Sensory bins filled with sand, water, or rice, along with tools like scoops and measuring cups, encourage exploration and hands-on learning. Coding toys like simple robots or puzzle mazes help develop problem-solving and logical thinking. Additionally, digital tools like educational apps and interactive whiteboards can enhance STEM experiences. Art supplies, such as colored pencils and paper, also play a role in fostering creativity and design skills. These materials are versatile and can be adapted to various STEM activities, making them invaluable for both classrooms and homes.